Distal Biceps Rupture

- Distal Biceps Ruptures are a fairly uncommon injury among throwers, more often occurring in middle-aged men (40-60) when an eccentric force is applied to a flexed and supinated (palms-up) forearm
** Eccentric Force = occurs when tendon is lengthening while the muscle is maximally contracting
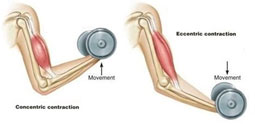
- The biceps muscle is made up of two distinct muscle heads in the upper arm working primarily to supinate (palms-up) the forearm as well as flex the elbow by inserting on the radial tuberosity
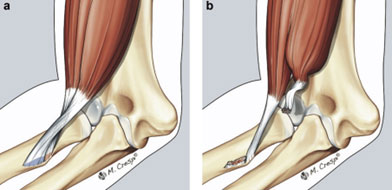
- Distal bicep injuries occur on a spectrum ranging from tendinosis (degeneration) to partial and complete ruptures where the tendon pulls off the radial tuberosity.
SYMPTOMS:
- Patients will often describe a sudden eccentric extension force applied to a flexed elbow leading to a “popping” or “tearing” sensation in the front of the elbow
- Complete ruptures may lead to immediate swelling and bruising around the elbow and upper arm as well as pain and weakness
- Partial tears may have less swelling and bruising but will typically experience significantly more pain than complete ruptures
- Both partial and complete ruptures will experience pain and weakness with forearm supination (palms-up) and elbow flexion
DIAGNOSIS:
- In cases of complete ruptures, the muscle belly may retract into the upper creating a reverse “Popeye deformity” or clinically obvious bulge in the arm
- The “hook test” uses the examiners index finger to hook or palpate an intact biceps tendon at the elbow going from lateral to medial
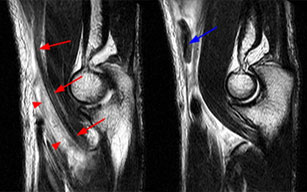
- X-rays are helpful to rule out any fracture or bony abnormalities. However, an MRI is the gold standard for identifying distal biceps ruptures
- MRI T2 Axial and Sagittal sequences can identify partial vs complete ruptures as well as the degree of retraction
TREATMENT:
- Treatment options are based on the degree of injury as well as patient’s activity levels
- The standard of care for a complete tear is early operative repair of the ruptured tendon
- In the case of a complete tear, patients treated non-operatively can expect significant reduction in supination strength and supination endurance (ex: turning a screwdriver) Pain is typically not a long-term issue with complete ruptures
NON-SURGICAL:
- Partial tears may be amenable to nonoperative treatment depending on the patient’s activity level and physical demands on the arm
- Nonoperative treatment includes allowance of full range of motion, NSAIDS, avoidance of weight lifting and return to activities as pain/weakness subsides
- Patients who are unable to return to activities or have ongoing pain and weakness should consider surgery
OPERATIVE:
- There are a number of reliable surgical techniques described to reattach the ruptured distal biceps to the radial tuberosity
- A combination of sutures, anchors, screws and buttons are typically utilized to affix the tendon to bone
- Tissue graft may be necessary in chronic cases or when the tendon has significantly retracted
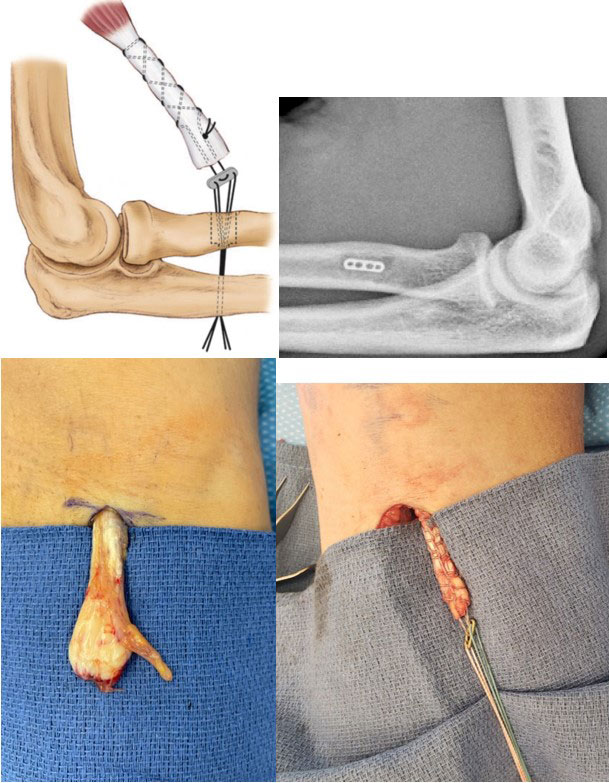
- Schematic demonstrating suture button sewn to end of biceps tendon and placed back to insertion site through radius
- X-ray demonstrating button placement against radius for attachment of biceps tendon
- Ruptured Distal Biceps Tendon with chronic thickening of tendon at insertion site
- Button sewn to healthy biceps tissue for repair
RECOVERY:
- Early elbow range of motion is implemented within the first two weeks following surgery
- Avoidance of active flexion and passive extension during the first 4-6 weeks to allow the tendon to heal
- Light resistance strengthening is initiated at 6-8 weeks with progression as tolerated and full return to normal activities at 3-4 months
- Return to play after rupture distal biceps reconstruction is typically 3-4 months after surgery when pain is minimal, and motion and strength has normalized