Capitellar OCD

- Osteochondritis Dissecans of the elbow or “Capitellar OCD” refers to a local disorder of subchondral bone that results in fragmentation of the smooth articular cartilage and underlying bone
- Most frequently seen across the lateral (outer) portion of the elbow at the end of the humerus called the capitellum
- The exact etiology of OCD is unknown. However, microtrauma secondary to repetitive valgus stress overload (throwing motion) across the elbow combined with poor blood supply is presumed to be the primary cause
- The combination of repetitive trauma with poor blood supply leads to weakened cartilage that cracks, separates and chips away
- Most often seen in baseball players and gymnasts between the ages of 12-17 years of age
- Typically responds well to nonoperative treatment in early stages but in advanced stages often requires surgery
***Panner Disease is an extremely rare condition also occurring in the humeral capitellum in adolescents. Thought to be a distinctly different condition from OCD affecting patients less than 10 years of age and typically self-limiting
SYMPTOMS:

- Adolescent throwers and gymnast typically present with pain across the lateral portion of the elbow
- Athletes often describe a vague discomfort associated with throwing or weightbearing activities
- In later stages, throwers may develop decreased elbow range of motion particularly loss of elbow extension
- Late findings may also present with mechanical symptoms such as catching, clicking or locking
- The differential diagnosis includes: (in order of prevalence)
- “Little Leaguer’s Elbow” (fragmentation of the medial epicondyle vs dissociation of medial epicondyle physis)
- Delayed closure of olecranon epiphyseal plate/olecranon stress fractures
- OCD lesions/Panner’s Disease
DIAGNOSIS:
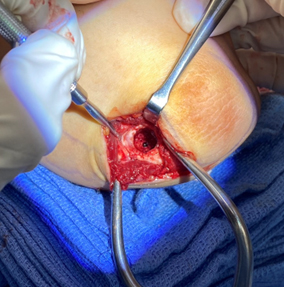
- Radiographs are used to detect the size, location and severity as well as skeletal age of the patient.
- Contralateral X-rays can help determine patients age as the affected side will have premature closure of the capitellum and radial head physes with delayed closure of the medial epicondyle and olecranon physes secondary to valgus stress overload


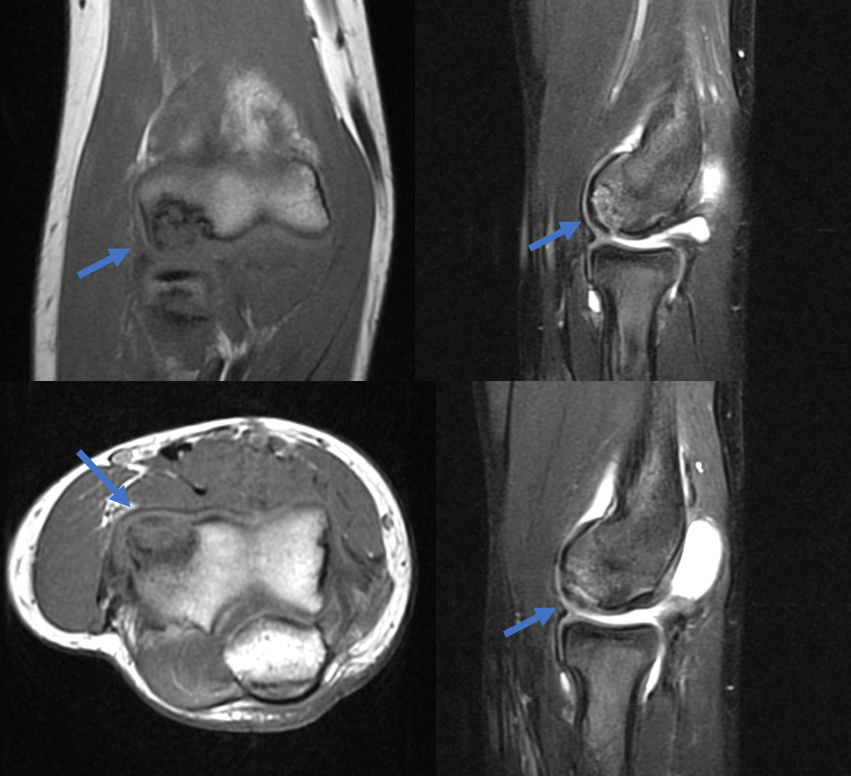
X-rays demonstrate a large lateral lesion within the capitellum consistent with an OCD lesion. The articular surface appears irregular
- Various classification schemes help determine severity. This includes:
- Grade I: Localized Flattening of articular cartilage
- Grade II: Nondisplaced fragmentation of the cartilage
- Grade III: Displaced or detached fragments/sclerosis or loose bodies
***Location of lesion on capitellum is important because lateral lesions tend to have inferior outcomes than central lesions
*** Throwing athletes tend to have more anterior lesions compared to gymnasts
- “Stable” lesions have been defined as those with open capitellar physis, localized flattening and radiolucency of subchondral bone with near normal elbow range of motion. Grade I is considered stable and Grade III is unstable. Grade II can be stable or unstable
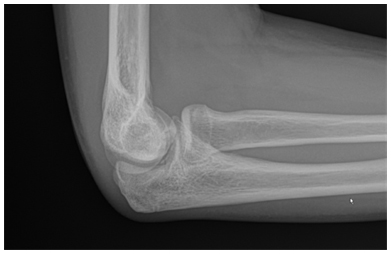
- MRI can help define stability of Grade II lesions
- Irregular contour or discontinuity of articular cartilage on MRI suggests unstable lesions
- CT scans and ultrasound can also help define size, location and stability of fragments
MRI demonstrates an unstable fragmented lesion within the capitellum
TREATMENT:
- Treatment is based on symptoms, physical examination (loss of motion/mechanical symptoms), size, location and stability of lesion
- Grade I stable lesions can typically be treated well with nonoperative measures
- Unstable lesions less than half the capitellum can generally undergo loose body removal and resection of unstable fragments
- Articular reconstruction with osteochondral autograft transplantation (cartilage transfer from donor area to affected area) is typically necessary for lesions larger than half of the entire capitellum
NONOPERATIVE:
- Local rest with avoidance of throwing while focusing on proper pitching mechanics
- Specifically assessing for scapular dyskinesia, hip or joint motion which can all be related to poor mechanics which increases valgus stress overload in the accelerations phase of throwing and has been associated with OCD lesions
- Even after players return to play, close attention to symptoms, function and x-ray findings must be followed until complete healing is achieved
SURGICAL:
- Surgical treatment is indicated for unstable capitellar OCD lesions
- Elbow arthroscopy or osteochondral autograft transplantation is chosen based on size of lesion and skeletal age
- Elbow arthroscopy is used for fragment excision, loose body removal and debridement for small unstable fragments
- Large unstable lesions in skeletally immature elbows are indicated for osteochondral autograft transplantation where cartilage can be harvested from a donor site (typically knee) and transferred to elbow lesion to restore normal healthy cartilage
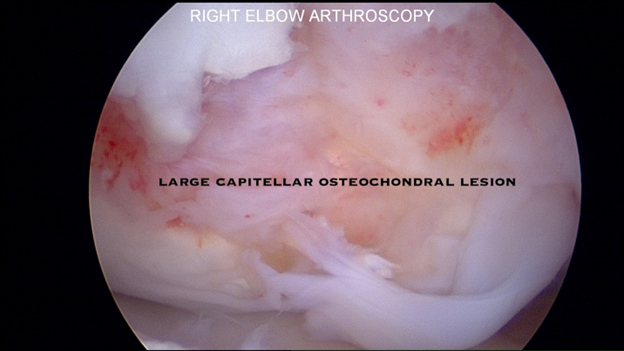
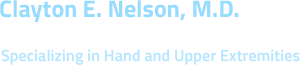
Arthroscopic examination of an OCD lesion
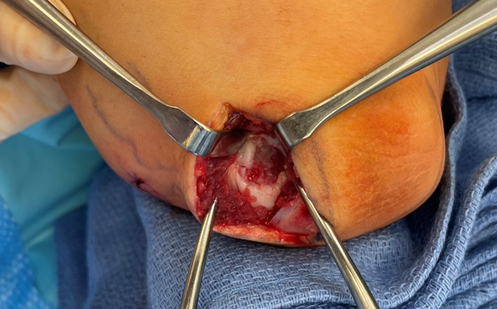
The damaged cartilage and underlying bone is removed using appropriate sizers

A size-matched plug of cartilage is harvested from the non-weightbearing portion of the knee and prepared for transfer to the elbow

The cartilage plug is contoured and placed within the elbow defect completing the cartilage transfer
RECOVERY:
- Full recovery and return to play is highly variable and based on multiple factors including patient’s age, treatment and level of activity. A combination of protected early range of motion with progression to strengthening and gradual return to sport specific play occurs over 6-18 months. Prognosis is based on early detection and physeal status.

Well healed osteochondral lesion of the capitellum at 1 year